Don’t let complex topics hold you back; Rapid Assignment Help delivers seamless and effective Assignment Help solutions.
Change is not just a choice in the dynamic environment of contemporary organisations; it is also a need. The need for reform is particularly pressing for the National Health Service or NHS in the United Kingdom, a sizable and crucial healthcare organisation servicing millions of people. This assignment examines a proposed transformation programme within the NHS critically. A thorough assessment of the leadership of strategic change, the impact of technological advancements, the application of management accounting techniques and the formulation of a change proposal are all required due to the organization's commitment to excellence in healthcare delivery and the need to adapt to a constantly changing healthcare environment. This project intends to address the difficulty of change management within such a complex, varied healthcare system, keeping in mind the NHS's ultimate objective to offer high-quality healthcare services to the nation. Within this framework, one can examine the urgent need for change as well as the approaches to deal with probable problems and obstacles to the implementation of change. The NHS's dedication to disciplinary expertise, knowledge and understanding of its chosen field comes to the fore as the voyage of discovery gets underway. This assignment aims to provide the NHS with the tools and insights required to thrive in the face of dynamic healthcare landscapes and to maintain its crucial role in the healthcare ecosystem through a critical analysis of change management, technology integration, financial implications and leadership strategies.
One of the biggest healthcare systems in the world, the National Health Service or NHS in the United Kingdom was established in 1948 and serves a population that is both varied and dynamic. Over 28 million individuals now have the NHS App in their pockets, over 40 million people have an NHS login and the majority of NHS trusts use an electronic patient record system (Gov.uk, 2023). The NHS has made significant progress, but it still functions in a healthcare environment that is changing all the time because of things like rising healthcare expenses, technology breakthroughs, shifting patient expectations and shifting legislation. In that case, the concerned organisation NHS is suggested to focus on developing telehealth services for the employees to improve the employees’ satisfaction. The NHS must embrace strategic change if it hopes to maintain its efficacy and agility.
The NHS is currently dealing with a slew of complex issues that, if left untreated, threaten its ability to provide high-quality healthcare and stimulate innovation. The rising expense of healthcare is a major problem. This increase in costs is principally driven by the ageing population and the rising prevalence of chronic diseases, both of which increase demand for healthcare services. According to The King's Fund's 2019 report, health spending increased by 1.2% yearly in real terms between 2010/11 and 2014/15 and a similar trend is expected until the end of the current parliament (Kingsfund.org.uk, 2023). Furthermore, the NHS is experiencing a technological lag. Despite significant progress in integrating digital health solutions, the country has struggled to completely embrace cutting-edge technologies. Integrating sophisticated technology, as proposed by recognised technology adoption models, is critical for boosting healthcare process efficiency and improving patient care. Another significant problem is responding to changing patient expectations, which necessitates a more patient-centric approach. Patients nowadays are well-informed, connected and proactive in their health management. Furthermore, the NHS functions in an ever-changing regulatory and policy environment. Noncompliance, as evidenced by several research on data privacy and healthcare law, risks legal and financial consequences. This change is critical given the expected 55% increase in the population of those over 85 by 2037, part of a continuing trend of population growth that outpaces comparable nations. Failure to respond to this demographic transition is expected to result in a 260,000 to 360,000 workforce gap by 2036/37 (England.nhs.uk, 2023). Compliance, data security and ethical healthcare practices all require adaptation to these changes.
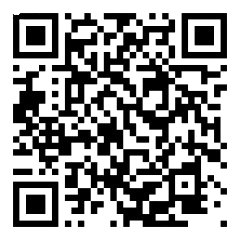
The case for change is strengthened by facts and theories that confirm the need for these changes. Based on the work of Michael Grossman and Kenneth Arrow, health economics theory emphasises the significance of investing in healthcare to improve individual and societal well-being (Yildiz, 2019). Adequate funding is required for the NHS to meet the growing demand for healthcare services, according to this view. Integrating sophisticated technology, as indicated by the Technology Acceptance Model or TAM and the Innovation Diffusion Theory, is consistent with technology adoption ideas (Harris and Rogers, 2023). This integration not only enhances the efficiency of healthcare services but also makes the NHS more patient-centric, in accordance with patient-centred care ideals.
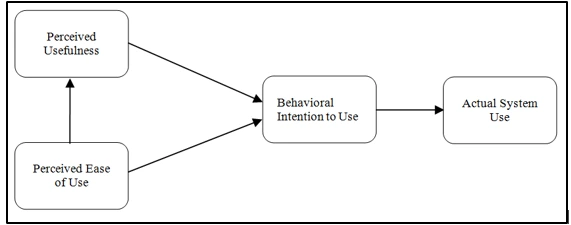
Figure 1: Technology acceptance model
A plethora of studies and analyses on data protection and healthcare regulation support the necessity for compliance with evolving regulations. Given the potential legal, financial and reputational ramifications of noncompliance, these sources emphasise the importance of adhering to standards for data privacy and ethical healthcare practices (Tartaro, 2023). Finally, the current status of the NHS emphasises the importance of transformation. Changing patient expectations, rising healthcare costs and altering legislation all need a deliberate response (Hays et al., 2020). The suggested change programme is built on a solid basis of health economics, technology adoption theories, patient-centred care principles and regulatory compliance. This effort attempts to solve these issues and secure the NHS's position as a forerunner in healthcare, providing quality care while adapting to the changing healthcare scene.
Large-scale change projects, such as those undertaken by the NHS, are analogous to running a marathon rather than a sprint. It necessitates a systematic and methodical approach, yet as with any long race, hurdles and impediments are unavoidable. This section digs into identifying potential problems and disruptions that may develop during the change project, explores how these issues may impact effective leadership and emphasises the need to deal with these concerns.
Potential Challenge: During any organisational transformation, resistance to change is an ever-present obstacle (Reed and McDermott, 2020). Employees and stakeholders may object to the proposed change because they are afraid of the unknown, have job instability, or are concerned about changes in their jobs or duties.
Impact on Effective Leadership: The effectiveness of change leadership can be undermined by resistance. It can result in implementation delays, lower employee morale and even open opposition. The success of the change initiative may be jeopardised if resistance is not addressed.
Significance: Recognising and addressing opposition is critical. It is consistent with the findings of Kurt Lewin's Change Management Model, which emphasises the need to 'unfreeze' the present state, allow change and ' refreeze' the new state (Mindtools.com, 2023)). Leaders must engage employees, communicate clearly and offer assistance to overcome opposition and build a positive change environment.
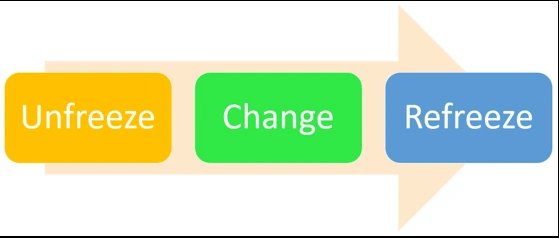
Figure 2: Kurt Lewin's Change Management Model
Potential Challenge: Inadequate or ambiguous communication can cause confusion and misalignment among stakeholders. Employees may be sceptical and uncertain if they do not grasp the objective, extent and benefits of the change.
Impact on Effective Leadership: Transparent and constant communication is required for effective leadership to accomplish telehealth services for employees (Kaul et al. 2020). Without clear communications, executives may struggle to get staff buy-in, resulting in misinterpretation and dissent.
Significance: Clear communication is essential in John Kotter's 8-Step Change Model, which emphasises the significance of developing and conveying a clear vision (Trawick and Carraher, 2023). Leaders should provide a compelling story outlining the objective and benefits of the transformation. Engaging in active and open communication channels builds trust and aids in the transition to a new environment.
Potential Challenge: Budget limits or insufficient staffing, for example, can provide substantial obstacles (Saville et al., 2019). Implementing change may necessitate more resources, putting existing finances and human resources under strain.
Impact on Effective Leadership: Resource restrictions can obstruct effective leadership by reducing the organization's ability to carry out the planned transformation programme. This can cause delays and impede the achievement of goals.
Significance: The Resource-Based View or RBV philosophy of strategic management is based on effective resource management (Collins, 2021). Leaders must plan how to distribute resources efficiently and prioritise areas that directly contribute to the success of the transition. Collaboration with financial and operational professionals is required to efficiently overcome resource limits.
Potential Challenge: Employees are frequently required to learn new skills or adapt to new processes as part of change programmes. Failure to offer proper training might result in skill gaps and poor performance.
Impact on Effective Leadership: Leaders must ensure that personnel have the essential skills and expertise to successfully implement the change (Mansaray, 2019). Failure to address skill gaps can stymie the pace of the change.
Significance: According to the Human Capital Theory, an organisation's investment in staff training and development is critical for long-term success (Bawono, 2021). Effective change management leadership necessitates identifying skill shortages and implementing focused training programmes to bridge them to accomplish telehealth services for employees. This investment not only helps the change but also improves the overall human capital of the organisation.
Potential Challenge: Cultural misalignment can arise when the current organizational culture does not support the proposed change (Asatiani et al., 2021). This misalignment can lead to resistance, confusion and a lack of motivation among employees.
Impact on Effective Leadership: Aligning the organisational culture with the desired change culture is required for effective leadership to accomplish telehealth services for employees. If this is not accomplished, the change attempt may face opposition and the change may fail to take root in the DNA of the organisation.
Significance: The Organisational Culture Model developed by Edgar Schein emphasises the importance of connecting the present culture with the desired culture for change (Ojogiwa and Qwabe, 2021). Leaders must comprehend the current culture, identify areas of misalignment and adopt tactics to remodel the culture to support the change endeavour. Finally, identifying possible challenges in a change project is an important stage in change management. Recognising these issues, addressing them and creating a climate that promotes successful change adoption are all part of effective change leadership to accomplish telehealth services for employees. From resistance to resource limits, each difficulty provides an opportunity for leaders to demonstrate their ability to navigate complicated transformation processes.
Implementing change inside an organisation as complicated as the NHS requires a well-thought-out approach in the ever-changing landscape of the healthcare sector. Leaders in the NHS must carefully examine various change techniques, bearing in mind both the LLSC principles and John Kotter's Eight Steps of Change. This section examines many techniques to change, focusing on the benefits and drawbacks of each.
| Change management stage | Actions | Proposed time |
| Create urgency: | Highlighting the benefits of telehealth | 2 months |
| Build a range, powerful coalition: | Assembling efficient team leaders | 3 months |
| Develop a vision for change: | Outlining clear roadmap | 3 months |
| Communicate the vision: | Engaging the stakeholders | 4 months |
| Remove obstacles: | Improving training to minimise skill gap | 3 months |
| Generate short-term wins: | Outlining previous examples | 3 months |
| Build on wins: | Highlighting the positive results | 4 months |
| Embade changes into culture: | Incorporating telehealth practices | 2 months |
Table 1: Kotter’s 8 Stage model for incorporating telehealth
An incremental approach to change implementation inside the NHS is one method. Leading Large-Scale Change emphasises a holistic approach to transformation, concentrating on change leadership qualities, contextual understanding and stakeholder engagement to incorporate telehealth services for employees (England.nhs.uk, 2023). This technique is consistent with the LLSC philosophy of "Plan, Do, Study, Act". Incremental deployment is gradually integrating telehealth solutions inside specific departments or regions of the NHS, with the goal of gradually scaling up over time.
Advantages: The advantage of incremental rollout is that it reduces disruption within the NHS. The progressive implementation of telehealth solutions allows employees and stakeholders to adjust to the changes at a controlled pace, decreasing opposition and potential churn (Edge, 2021). It also promotes adaptive learning because the organisation may take useful lessons from one step and apply them to the next. Furthermore, the progressive implementation provides for better-controlled cost management because resources may be allocated depending on the success and demands of each step, avoiding waste.
Disadvantages: The delayed realisation of the full benefits of telehealth, on the other hand, is a key disadvantage of this method. Patients may not benefit as rapidly from remote healthcare, thus delaying gains in patient care and cost savings (El-Tallawy et al., 2020). Coordinating several phases of implementation is time-consuming and requires precise preparation and interdepartmental collaboration. Staff and patients may view this strategy to be weak in commitment to change, which could lead to scepticism and delayed adoption.
A comprehensive rollout strategy is beneficial for improving the healthcare system. In this method, the NHS rapidly implements telehealth technologies across the organisation, with the goal of universal adoption and integration. This approach prioritises a quick transition.
Advantages: A robust rollout strategy provides the benefit of faster advantages. The rapid implementation of telehealth technologies can lead to significant improvements in efficiency and patient care (Gajarawala and Pelkowski, 2021). It demonstrates a strong commitment to change, which may gain support from stakeholders, which is critical in a large-scale transformation. Furthermore, a complete rollout facilitates telehealth system integration by centralising and standardising the process, eliminating compatibility difficulties.
Disadvantages: Regardless of the benefits, quick change might lead to greater resistance from employees who may feel overwhelmed by the move. This opposition can jeopardise the successful implementation of telemedicine solutions. Furthermore, the rapid pace of adoption may lead to missed details and significant faults in the implementation process, resulting in setbacks (Osaba et al., 2021). Ensuring that all personnel receive proper training in a timely manner can sometimes be a logistical difficulty.
The technique of building a public-private collaboration is consistent with the LLSC principle of "Collaborate and Build Consensus" as well as Kotter's fifth step of "Enable Action by Removing Barriers"(Nhselect.nhs.uk, 2023). The NHS engages with private telehealth companies in this approach to use external expertise and resources.
Advantages: Access to external expertise is a significant benefit of the public-private partnership method. Collaboration with private telehealth companies enables the NHS to harness specialised knowledge and resources, hence accelerating adoption. Sharing costs with a private partner can also assist the NHS in managing the financial load associated with technological transformation. It also reduces the NHS's burden by mitigating some risks, such as data security and technology updates, which the commercial partner may take on.
Disadvantages: This strategy, however, is not without difficulties. Concerns about data security and privacy can arise when patient data is shared with private businesses. If the cooperation proves to be costly in the long run, the NHS's financial sustainability may be jeopardised. Furthermore, collaborating with external entities may result in a loss of control over the path of change, potentially leading to decision-making conflicts.
Pilot programme execution is consistent with the LLSC principle of "Learn and Adapt". This strategy entails conducting small-scale telehealth experiments in specific regions or departments to test feasibility and impact prior to general introduction.
Advantages: Pilot programmes offer the benefit of risk reduction. The NHS can analyse potential obstacles and issues on a smaller scale by undertaking small-scale trials, lowering the likelihood of a large-scale failure. Pilot programme data and insights provide evidence-based decision-making, ensuring that the overall implementation plan is well-informed (Saha et al., 2023). Staff and patients participating in pilot programmes can help to generate support for the larger change endeavour.
Disadvantages: On the other side, the NHS may not realise the full benefits of telehealth until later in the adoption process, thus postponing cost reductions and care improvements. Managing pilot programmes in different regions or departments necessitates careful coordination and communication, both of which can take time. Furthermore, insights from pilot programmes may not completely coincide with bigger goals, potentially leading to decision-making conflicts.
The hybrid model mixes in-person and remote care to improve the health system (Assets.publishing.service.gov.uk, 2023). Patients and healthcare professionals can select between traditional in-person care and telemedicine under this strategy, which provides a balanced approach to change.
Advantages: The fundamental advantage of the hybrid approach is its adaptability. Patients and healthcare professionals can opt for either traditional in-person care or telemedicine, providing a balanced approach to change. This adaptability appeals to both traditionalists and telehealth supporters, lowering resistance to change. Patients benefit from a combination of in-person and telehealth services, which allows them to access a wider range of care options.
Disadvantages: Nonetheless, this strategy may pose coordination issues. Coordination of the hybrid care model and maintaining seamless technology integration can be difficult and time-consuming. Inefficiencies in resource allocation and patient care may result from balancing the use of in-person and telehealth services, thereby raising operating expenses for the NHS.
Understanding the financial implications of organisational change is a vital component of the decision-making process. A comprehensive financial study evaluates not just the costs and advantages of the proposed change, but also how the change would affect both income and capital budgets over a multi-year period. This part goes into the complexities of financial analysis, employing management accounting methodologies to generate a range of financial results. Such analysis is critical for sound decision-making and a long-term change project.
Before embarking on any transformation programme, it is critical to do a thorough financial analysis. This process begins with a cost-benefit analysis of the proposed modification. These expenses could include expenses for technology acquisition, training, employee modifications and other necessary infrastructure improvements. These costs must be identified and quantified as part of the financial appraisal process.
Figure 3: Tool: Driver diagrams
Consider the following scenario: a hospital has set a Large-Scale Change or LSC target to reduce costs by 6% in the current year by enhancing quality (England.nhs.uk, 2023). Such a hospital is motivated by expanding its money-related assets and making strides in the quality of healthcare administrations. This serves as an illustration of the financial results of the alter. To determine the feasibility and desirability of the change proposal, the costs of adopting quality improvement methods, training and relevant technology must be evaluated against the anticipated cost savings.
A thorough financial analysis must investigate the impact of the proposed change on both the income and capital budgets. When analysing revenue, it is critical to predicting how suggested changes would affect income streams. The goal of cutting expenses while enhancing quality has clear ramifications for income in the instance of the aforementioned hospital (Waitzberg et al., 2022). It could entail forecasting greater revenue as a result of improved services, additional offerings, or cost reductions. Organisations, on the other hand, must account for any potential income reductions, particularly if there is an initial decrease in production or capacity during the transition phase. Capital budgets include cash allocated for long-term investments and the proposed shift may entail considerable changes in this area. Capital expenditures for technological upgrades, facility improvements, or quality improvement activities may fall into this category. In the case of this hospital, the effects on the capital budget could be significant, as investments in technology and infrastructure enhancements are likely to be necessary to reach the quality and cost-cutting targets.
The financial evaluation process mainly relies on management accounting approaches to give clarity and precision. In the context of the hospital's LSC goal, cost-benefit analysis is critical for assessing the financial implications of quality improvement programmes. It enables organisations to compare the costs and benefits of a proposed change in an organised manner, assisting decision-makers in determining the feasibility and potential return on investment. Budget forecasting tools such as trend analysis and scenario planning provide insight into potential financial outcomes over multiple years. In this hospital example, scenario planning is extremely useful. This is essential for a hospital looking to cut costs while improving quality since it enables the organisation to simulate many scenarios while taking into consideration various variables, risk factors, and external economic realities.
In particular for a hospital aiming to reduce costs while increasing quality, a financial evaluation is not complete until a range of prospective financial outcomes is presented. This plan accounts for the unanticipated events and possible hazards that could impact the change endeavour, like modifications to patient volume, payment schedules, or delays in the rollout of new technology. By offering a variety of potential outcomes, organisations can better prepare for the unexpected and create backup plans (Gurr and Drysdale, 2020). Additionally, it promotes more educated discussion among concerned parties, enabling them to decide based on knowledge about the proposed change and the hospital's financial stability. Since it provides a thorough understanding of the costs, viability, and prospective outcomes, the financial analysis is an essential component of managing change projects. A real-world example of the value of financial analysis in decision-making is the scenario of a hospital striving to decrease costs while improving quality. For transformation programmes to be financially viable and sustainable over the long term, this type of analysis calls for both financial expertise and strategic thought.
| Year | Financial Implications | Income Budget (Millions) | Capital Budget Changes (Millions) |
| Year 1 | Cost-Benefit Analysis | $200 | $50 |
| Year 2 | Scenario Planning | Best-case: $206, Worst-case: $194, Most likely: $200 | Adjusted based on the chosen scenario. |
Table 2: 2-year Budget Plan
Get assistance from our PROFESSIONAL ASSIGNMENT WRITERS to receive 100% assured AI-free and high-quality documents on time, ensuring an A+ grade in all subjects.
Any significant change programme inside the NHS or any large-scale organisation must identify and address potential impediments to successful implementation. This section covers potential challenges, methods and solutions for overcoming them, as well as the crucial importance of good change management, building on insights from the "Marathon Effect."
Resistance to Change: Change frequently elicits resistance, which is a typical human reaction to the unfamiliar. Resistance can emerge at numerous levels in a complicated and established organisation like the NHS, from frontline personnel to high-level management.
Lack of Alignment: Misalignment between the change initiative with the NHS's current culture, beliefs and practises can be a major impediment. It could lead to a schism between the proposed change and the NHS's long-standing practices.
Resource Constraints: Limited resources, both financial and human, can impede the successful execution of the change endeavour. A lack of critical resources may stymie progress and limit the breadth of the endeavour.
Inadequate Communication: Among stakeholders, poor or insufficient communication can result in misunderstandings and confusion. To develop understanding and trust, communication must be open and straightforward.
Change Fatigue: Change initiatives at a big organisation like the NHS could feel endless. Employees may develop wearyness of ongoing change attempts as a result, which could affect their involvement and receptivity.
Effective Change Leadership: The leadership group must steadfastly drive the transition by outlining a compelling vision and exhibiting their dedication to accomplishing telehealth services for employees. The Marathon Effect, which emphasises that strong leadership is necessary to maintain momentum, is consistent with this method (Crowe-associates.co.uk, 2023).
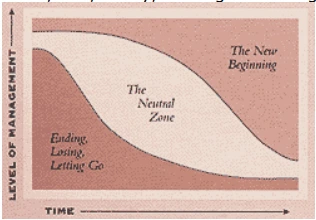
Figure 4: THE MARATHON EFFECT Change Champions:
Within the organisation, find and support change champions. These people can act as supporters of the change, highlighting its advantages and assisting in overcoming opposition.
Comprehensive Communication: Create a well-thought-out communication strategy to make sure that everyone involved is aware of the progress, justification and advantages of the change. The Marathon Effect emphasises the need for constant communication to maintain participant motivation.
Resource Mobilization: Make sure resources are available for the change endeavour and distribute them strategically. Redistributing employees or changing budget priorities may be necessary to support the endeavour.
Customized Training: Offer employees specialised training programmes to give them the tools they need to handle the changes. This approach supports the Marathon Effect's focus on the importance of education for successful change management.
The Marathon Effect is a theory that emphasises the value of persistent work and attention in achieving a long-term objective. It works well as an analogy for the reform initiative in the NHS.
Sustained Leadership: A change initiative demands enduring leadership, just as a marathon requires persistent dedication. The goals of the change are consistently inspired and guided by effective leaders.
Incremental Progress: Marathons are not won in one bound but rather by steady, gradual advancement. Similar to this, transformation programmes frequently contain multiple minor successes that boost their overall success.
Training and Preparation: Training and education are two ways that runners get ready for marathons. Employees also need training and planning to successfully adjust to changes.
Momentum Maintenance: Maintaining momentum is critical in a marathon. Consistent communication and assistance are required in change management to maintain the momentum of the change endeavour.
Resilience: Marathon runners face obstacles, but their perseverance keeps them going. Resilience is essential in change projects for overcoming obstacles and moving forward.
A successful change endeavour within the NHS relies on effective change management. It contains several crucial components:
Leadership: The tone of the organisation is set by effective leadership. Leadership not only starts but also guides change through various stages.
Engagement: It is critical to involve all stakeholders, from employees to leaders. The Marathon Effect emphasises that engaged individuals are more likely to stick with the change over time.
Communication: Clear and consistent communication aids stakeholders in understanding the objective, progress and advantages of the change. Marathon runners in The Marathon Effect must communicate well in order to coordinate their efforts.
Adaptability: Adapting to unanticipated problems and implementing lessons learnt are all part of change management. Overcoming obstacles requires flexibility and adaptability. Consequently, a thorough comprehension of potential roadblocks, a dedication to strategies and solutions and a knowledge of the Marathon Effect's guiding principles are all necessary for the successful implementation of a change project in the NHS. The NHS may successfully overcome these obstacles and reap the long-term advantages of the suggested transformation by placing a strong emphasis on leadership, communication, participation and adaptation.
In order to maintain its effectiveness and adaptability in the constantly changing healthcare environment, the National Health Service is facing numerous problems that call for a deliberate response. The main goal of this change plan is to address the urgent problems of rising healthcare costs, technological lag, shifting regulations and changing patient expectations by implementing a transformational leadership style (Webb, 2019). This strategy supports the NHS's primary goal of offering the country high-quality healthcare services. The NHS is going to be given the tools it needs to embrace change, encourage innovation and develop resilience as it negotiates the complexity of the healthcare ecosystem with the help of transformational leadership.
This leadership approach focuses on inspiring and motivating staff members through the development of a compelling vision, support for innovation and a focus on both individual and group growth. In the context of the NHS, this strategy comprises developing a vision for a flexible, cutting-edge and patient-centred healthcare system that fits in naturally with the NHS's primary goal of offering high-quality healthcare to the country. Additionally, it fosters intellectual stimulation, encouraging innovation and creativity to close technical gaps and meet changing patient expectations (Santarsiero et al., 2023). The key to addressing employee concerns and easing their transition to new procedures and technology is personalised consideration, which translates into customised training and skill development programmes.
Leadership Development: The NHS must strengthen its leadership capabilities in order to implement transformative leadership. This would entail mentoring, leadership development programmes and spotting and developing the organization's future transformative leaders.
Vision Articulation: Make the transformation of the NHS seem convincing. In order to handle the issues of rising healthcare expenditures, technology improvements, changing patient expectations and altering legislation, this vision should emphasise innovation, patient-centric care and adaptability (Stegemann et al. 2023).
Communication: Make sure that the organization-wide communication of the vision is clear and consistent. Various stakeholders, including frontline healthcare workers, office personnel and outside partners, should get customised messages.
Employee Engagement: Employees at all levels should be involved in the transformation process. Encourage them to contribute ideas, express concerns and actively engage in decision-making. This would instil a sense of ownership and dedication to the change.
Training and Skill Development: Provide focused training and skill development programmes to staff in order to meet their requirements as they adjust to new processes, technology and patient-centric care models. This should be tailored to each individual's role and duties.
Innovation Culture: Encourage an innovative and continual improvement culture inside the NHS. Encourage staff to try new approaches and technologies, as well as to recognise and reward innovative ideas and solutions.
Monitoring and Adaptation: Monitor the progress of the change initiative on a regular basis. Prepare to adapt and correct course as needed, addressing any impediments or opposition that may arise throughout implementation.
A well-defined action plan is required to effectively deploy transformational leadership inside the NHS. This approach includes introducing employee engagement efforts during the first three months, implementing leadership development programmes within the first six months and assuring vision articulation and communication within the first three months. Furthermore, personalised training programmes should begin within the first six months of the change effort and an innovative culture should be nurtured continually throughout the change project. Finally, a dedicated monitoring and adaption team with continuing resource allocation should be developed to ensure the initiative's success.
The chosen transformational leadership strategy is highly aligned with the NHS's key organisational aims. It immediately strengthens the nation's commitment to providing high-quality healthcare services by aggressively promoting patient-centred care through innovation and adaptation. Furthermore, the emphasis on innovation and continuous improvement is positioned to play a critical role in efficiently managing healthcare costs, guaranteeing efficient resource allocation and aligning with the goal of cost management (Molinaro et al., 2022). Furthermore, the method empowers the NHS to manage changing legislation in a proactive manner, ensuring compliance and ethical healthcare practices. Finally, by emphasising employee engagement, personalised training and skill development, the transformational leadership approach directly adds to the well-being and job happiness of NHS employees, furthering the goal of maintaining a motivated and highly competent workforce. The transformational leadership strategy effectively addresses NHS difficulties through visionary inspiration, innovation promotion and a focus on growth and resilience. Strategic change is ensured through a comprehensive execution plan, resource allocation and goal alignment.
Conclusion
In conclusion, the NHS transformation proposal is a critical endeavour aimed at addressing immediate financial challenges while setting the organisation for long-term growth and adaptation. The NHS's dedication to an organised, phased approach with a clear schedule, resource allocation and alignment with organisational goals demonstrates a deliberate transformation strategy. Recognising the inherent impediments to successful implementation, the plan emphasises effective change management methods based on the "Marathon Effect." Resistance to change and resource restrictions are overcome using tactics such as leadership, change champions, extensive communication, resource mobilisation and customised training, which collectively ensure that the change project stays on track. The Marathon Effect offers a strong comparison in the context of change management, highlighting the significance of consistent leadership, slow but steady progress, training and preparation, momentum maintenance, and resilience. It emphasises the idea that transformation is a marathon that requires unwavering commitment and focus. Effective change management is the cornerstone of this idea because it acknowledges the importance of leadership, involvement, communication, and adaptation in overcoming challenges and attaining long-term success. By implementing these suggestions, the NHS would be able to manage its current financial problems as well as foster a culture of flexibility, resilience, and ongoing improvement. This reform initiative is a critical step towards ensuring the NHS's financial stability and competitiveness in the rapidly evolving healthcare industry and, ultimately, the provision of high-quality healthcare services to all.
Reference
Introduction - Amazon's Workplace Change Management: A Strategic Analysis Get free samples written by our Top-Notch subject...View and Download
Introduction Ensure originality with Plagiarism-Free Assignment Help Solutions, providing well-researched, properly cited work...View and Download
INTRODUCTION Get free samples written by our Top-Notch subject experts for taking online Assignment...View and Download
Introduction Get free samples written by our Top-Notch subject experts for taking online Assignment Help services. In...View and Download
Introduction Get Free Online Assignment Samples from UK's Best Assignment Help Experts to boost your academic...View and Download
1. Introduction Get free samples written by our Top-Notch subject experts for taking online Assignment...View and Download
Copyright 2025 @ Rapid Assignment Help Services
offer valid for limited time only*