Choose Rapid Assignment Help for innovative, student-focused Assignment Help that caters to all your academic needs.
A country's healthcare systems are vital to the health of its populace. The effectiveness and efficiency of a nation's healthcare system can have a significant influence on a number of factors, including life expectancy, economic development, and overall standard of living. Using economic principles as a framework, the objective of this essay is to critically evaluate Ireland's healthcare system. Understanding its operation, the existing payment system, the workings of the market, and the ways in which these factors impact Irish health outcomes are the main objectives. Ireland's healthcare system has been praised and criticised over the years, often being contrasted with other European models. Modern medical technology and highly qualified medical workers may be found in Ireland, a developed country in the West. However, an analysis of the system's architecture has uncovered several intrinsic challenges that may compromise its effectiveness. In the sections that follow, this essay will look at the basic economic components of the Irish healthcare model, highlighting both its benefits and drawbacks.
Population and Demographics
When compared to other European nations, Ireland's population is very youthful. Recent research indicates that over 40% of the population is less than 30 years old, which presents both opportunities and challenges (Ivanković et al., 2022). Younger populations can result in a more dynamic labour force, but they also call for investments in family support, career options, and education.
Disease Burden
Although the death rates from a number of major diseases have decreased in Ireland, the nation still has to contend with diseases linked to a poor lifestyle, such as diabetes, heart disease, and obesity (World Health Organization, 2020).
In addition to the rising prevalence of non-communicable diseases, Ireland has problems with public health such as:
Life Expectancy: As previously shown, women's life expectancy in Ireland is 84.4 years, while men's life expectancy is 80.8 years (Statista, 2023). This demonstrates how healthcare services have improved and how the burden of sickness has decreased in many locations.
Morbidity and Mortality Rates: Notably lower death rates from diseases such as cancer, heart disease, stroke, and respiratory disorders point to successful medical treatments. But as said, compared to other European peers, the death rate from disorders of the respiratory system, including various malignancies, is noticeably greater.
Years of Life Lost (YLL): YLL is a statistic used to calculate early death. It can be assumed that the YLL has decreased in Ireland given the dropping rates of early mortality from major diseases. Even said, conditions with greater death rates, such as respiratory system disorders, may still play a major role in YLL (Vítězslav Jiřík et al., 2023).
Quality of Life: 82.1% of Irish people consider their health to be good or very good, reflecting the majority's favourable perception of their health (Colwell, 2021). A good quality of life in terms of health is reflected in this high self-perceived health status. The disparity in health perception according to income, however, suggests that health-related quality of life may differ among various socioeconomic groups (Wallander et al., 2019).
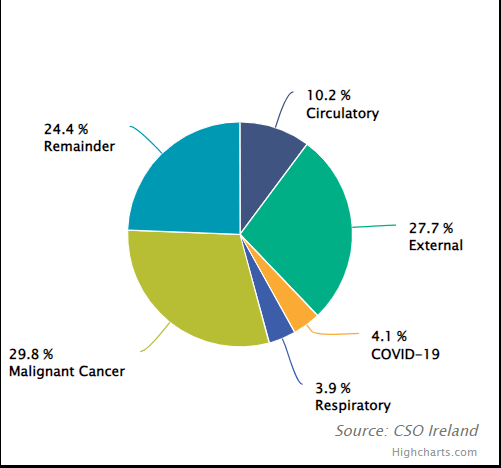
Figure 1: Causes of death in ireland
(Source: Cso.ie, 2022)
2,343 deaths (1.8 per 1,000) were attributed to circulatory system diseases, which include heart and blood vessel disorders (WHO, 2021). The majority of these deaths (1,065) were caused by ischemic heart disease (IHD), which is characterised by a reduced blood supply to the heart muscle and is frequently the result of coronary artery diseases. 373 deaths were attributed to cerebrovascular diseases, which are primarily conditions like strokes that result from problems with blood supply to the brain.
Ireland has a relatively small yet highly educated and competent labour force despite having a population of 5.0 million (Wright, 2022). The population size allows for more flexible and focused policy actions in the economic and public health domains. A robust economy is indicated by a GDP (Purchasing Power Parity) of $566.7 billion (Imf.org, 2019). This suggests a high degree of economic output and a rich economy, especially considering Ireland's small population.
Unemployment: Considering the state and difficulties of the world economy, a 5.6% unemployment rate is rather low. The majority of people in the working age population appear to be gainfully employed, which is crucial for the stability and expansion of the economy. Ireland's spending on healthcare increased significantly from 18.3 billion euros in 2011 to 30.5 billion euros in 2022 (Larkin et al., 2022). This substantial increase in just ten years demonstrates the nation's dedication to enhancing healthcare services, access, and infrastructure.
Year-over-Year Growth: as per the details of OECD (2022), 6.6% growth in healthcare spending from 2021 to 2022 demonstrates the nation's ongoing emphasis on healthcare, which may be due to rising demand, advancing technology, or inflationary pressures.
Current vs. Capital Expenditure: Although current spending accounted for a sizable portion (95%) of healthcare spending in 2021, since it was needed for urgent medical needs and services, it is noteworthy that capital spending increased thrice between 2012 and 2021. This spike in capital expenditures points to significant outlays for long-term healthcare infrastructure, such as new medical facilities, equipment, and technology.
Ireland has a dual healthcare system that provides its citizens with access to both public and private medical care.
Public Healthcare System
Regulation and Establishment: Ireland's public healthcare system is governed by the Health Service Executive (HSE), which was founded in accordance with the Health Act of 2004. A range of services are offered by the public healthcare system, such as hospital inpatient and outpatient care (International Trade Administration, 2022).Holders of Category I medical cards are entitled to free primary and acute care services.For public patients, there is no cost for diagnostic procedures like X-rays or lab testing. Spending and Budget: Ireland's 2022 health budget is projected to be €21 billion (Charlesworth et al., 2021). The central government provides a significant portion (about 78%), indicating the government's commitment to and priority for healthcare.
Private Healthcare System
Healthcare organisations and individual medical experts make up the private healthcare sector. In contrast to the public system, patients typically pay the whole cost of services offered. Many Irish people choose private health insurance, which can pay for a sizable amount of private medical bills, to help with the costs of private healthcare (Irishlifehealth.ie, 2022). The private healthcare system is a valuable addition to the public one, frequently enabling quicker access to specialists and specific procedures, as well as services and luxuries that may not always be easily available in the public sector.
Implications
Approximately one million individuals are served by each area in Ireland. The provision of services extends beyond official bodies and encompasses a combination of public, volunteer, and private suppliers (Health.ec.europa.eu, 2021). The inclusion of a diversified assortment of professionals guarantees the availability of a broad spectrum of services and areas of expertise throughout the nation. The implementation of a dual system guarantees the provision of healthcare services to individuals of all backgrounds, hence promoting accessibility (Ivanković et al., 2022). While the public system gives vital services at a reduced or free cost, the private system provides expedited and occasionally more specialised healthcare for individuals with the financial means to access it.
The coexistence of both systems has the potential to enhance the quality of healthcare, since each sector contributes its unique characteristics. The economic impact of the healthcare industry is multifaceted. On one hand, the public system plays a crucial role in providing widespread coverage. On the other hand, the private sector, with its range of services, also makes a substantial contribution to the economy (Riordan et al., 2021). Finding a delicate balance between the two systems so that the accessibility and quality of public healthcare are not negatively impacted in comparison to private healthcare is one of the issues (Kentikelenis and Stubbs, 2021).
The healthcare system in Ireland is distinguished by its dual structure, encompassing both public and private healthcare options. The Health Service Executive (HSE) is in charge of running the public healthcare system. The country allocated €21 billion for health in 2022, with the main goals being to reduce waiting list backlogs in acute hospitals and enhance the help given to people with disabilities (Thomas, Poku-Amanfo and Patel, 2022). Additionally, the administration has designated free contraception as one of its primary areas of priority for women's healthcare services.
Although the population of Ireland is quite large, behavioural risk factors including obesity and smoking are nevertheless causes for concern (Hruby and Hu, 2015). Although healthcare quality is typically high, the ability to receive treatment may be impeded by financial constraints and lengthy waiting periods. The healthcare system comprises various components, including acute care, primary care, continuing care, and community care services. These services address a wide range of health-related needs, such as mental health, impairments, and family welfare (World Health Organization (WHO), 2022). Both public and private healthcare providers play crucial roles in the delivery of healthcare services.
The healthcare infrastructure in Ireland comprises a combination of publicly and privately owned hospitals, whereas public hospitals cater to patients from both the public and private sectors. Upon admittance to public hospitals, patients are presented with the choice to pick for either public or private treatment alternatives (Colombo and Tapay, 2021). The nation accommodates a total of 48 publicly funded hospitals, which are categorised into seven distinct hospital groups. Additionally, there are 21 privately owned hospitals that are connected with the Private Hospital Association (PHA). In the year 2021, the nation of Ireland has a ratio of three hospital beds per 1,000 individuals (HMI, 2023). As cited by Stepovic et al., (2020), in the year 2020, the proportion of gross domestic product (GDP) allocated to total health expenditure was recorded as 7.2%, which was marginally lower than the average of 9.9% observed across the European Union (EU).
The Sláintecare Implementation Strategy and Action Plan 2021—2023 was unveiled in May 2021 with the objective of transforming Ireland's existing two-tier health system into a universal healthcare model similar to the National Health Service (NHS) in the United Kingdom. The objective of the plan is to optimise the experiences of patients and clinicians, mitigate healthcare expenditures, and boost overall outcomes. According to the Irish College of General Practitioners (ICGP) details by Collins and Homeniuk, (2021), there are an estimated 3,496 active general practitioners in Ireland, and there exist robust linkages between the healthcare sectors of Ireland and the United States.
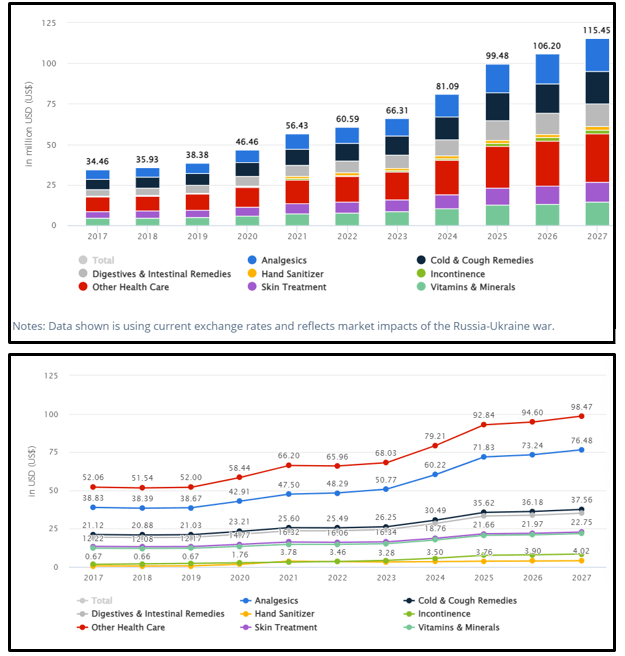
Figure 2: Revenue in the Health Care market
(Source: Statista, 2022)
The projected expansion of the healthcare industry in Ireland is estimated to be 14.85% between the years 2023 and 2027, with the potential to attain a market value of US$115.40m by the end of 2027 (Statista, 2022). According to forecasts of Ibisworld, (2023), it is anticipated that the healthcare eCommerce sector in Ireland will generate revenues of US$66.3m by the year 2023. This projection indicates a growth rate of 9% compared to the previous year.
Get assistance from our PROFESSIONAL ASSIGNMENT WRITERS to receive 100% assured AI-free and high-quality documents on time, ensuring an A+ grade in all subjects.
According to the 2022 World Index of Healthcare Innovation, Ireland shown notable progress by ascending from its previous rankings of 4th in 2021 and 5th in 2020 has to secure the 2nd spot. The score of the nation under consideration was recorded as 60.04, with Switzerland being the only country to get a higher score of 66.56 (Kelly and Young, 2017).
The principal source of financial support for the healthcare system in Ireland is derived from the government. The remaining monies are derived from voluntary healthcare contributions and household expenditures, with a substantial proportion going towards hospitals and ambulatory healthcare services. The prevalence of health insurance in Ireland is steadily rising (Cawley et al., 2021). As of the conclusion of 2021, the number of individuals receiving health insurance reached 2.4 million, representing approximately 47.1% of the total population. Moreover, it is worth noting that a significant proportion, approximately 40%, of the population in Ireland get medical services without incurring any direct expenses through the utilisation of the Category 1 or "Irish Medical Card" entitlement.
The period following the 2008 global financial crisis witnessed a considerable volatility in Ireland's healthcare expenditure. This might be attributed to the proactive measures undertaken by the administration to achieve economic stability and mitigate the repercussions of the crisis.
Selective Downsizing: The budget cuts were not uniformly allocated across all sectors within the healthcare industry. However, the government has discovered an imbalance in the ratio of nurses to doctors and other healthcare workers (Nolan et al., 2020). As a result, the funding cuts had a greater negative impact on nurses and midwives.
Reduction in Capital Expenditure: There was a significant decrease in the allocation of capital expenditure towards the healthcare sector, resulting in a direct impact on the infrastructure and developmental capacities of the healthcare system. The observed decline aligns with the prevailing governmental tendency to curtail diverse functions in the aftermath of a disaster.
There are several concerns that need to be addressed. Concerning Equitable Access: The recurring pattern of healthcare expenditure, particularly its decline during periods of economic recession, has prompted concerns over the availability of healthcare services, particularly for socioeconomically disadvantaged populations (Teja et al., 2020). Concerns arose over the potential exacerbation of economic disparities and the potential detriment to the welfare of less affluent households due to these expenditure trends.
The increase in private health insurance contributions towards healthcare finance was observed as the government faced the challenges of the financial crisis and explored strategies to restrict public expenditure. As cited by Sánchez Recio et al., (2022), the increase in demand can also be attributed to the implementation of prescription charges for those with medical cards, decreases in dental care benefits for this population, and the imposition of elevated user fees for various outpatient services.
The private sector's financial contribution to the healthcare sector reached its highest point in 2013, accounting for around 30% of the total expenses (Smith et al., 2021). Nevertheless, as the economic conditions began to improve, the aforementioned proportion experienced a decline of 4 percentage points by the year 2019.
The stability of household out-of-pocket payments in relation to healthcare expenses experienced nominal yearly growth of less than 1% in the five years preceding the onset of the pandemic.The Impact of the Pandemic on Private Health Financing The financial load on individuals in this context is comparatively lower in relation to several other countries within the Organisation for Economic Co-operation and Development (OECD), therefore highlighting a diminished level of financial strain (Gori and Luppi, 2022).
The COVID-19 pandemic presented unparalleled difficulties, necessitating an increased involvement of the state in health financing. Consequently, the proportion of private contributions experienced a further decline (Filip et al., 2022).
Healthcare financing in Ireland is a multifaceted system that involves a combination of public and private funding sources. These mechanisms are specifically designed to guarantee individuals' access to vital medical treatments while also addressing the issue of costs. The fundamental basis of this system is rooted in tax-based financing, wherein the Irish government predominantly relies on general taxes to finance the majority of healthcare services offered by the Health Service Executive (HSE) (Connolly and Wren, 2019). This technique guarantees a comprehensive and extensive stream of income to sustain a variety of healthcare requirements.
Although the primary objective of the public healthcare system is to offer extensive coverage, it is fairly uncommon for co-payments, such as outpatient prescription fees, to be required. Nevertheless, Connolly, (2023) mentioned that it is common for these fees to be subsidised, particularly for disadvantaged population groups, such as individuals with medical cards, in order to ensure that individuals facing financial difficulties can still receive these services despite their inability to afford the complete expenses.
The implementation of the medical card system in Ireland exemplifies the nation's dedication to ensuring equal access to healthcare services (Connolly, 2023). It provides a variety of medical services at no cost to eligible individuals, thereby ensuring that financial limitations do not hinder their access to necessary healthcare.
In addition to the public healthcare system, voluntary health insurance serves as a complementary resource, enabling individuals to avail themselves of private healthcare providers, faster medical attention, and consultations with specialists in both public and private hospitals. The implementation of health insurance levies has been undertaken in order to establish equity and standardise premium rates across policyholders (Domapielle, Akurugu and Derbile, 2021). Notwithstanding the implementation of these procedures, there continues to be a prevalence of out-of-pocket expenditures for diverse healthcare services, including consultations with primary care physicians, dental treatments, and certain pharmaceuticals. The approach aims to achieve a harmonious equilibrium between cost-sharing and the prevention of financial deterrents that may dissuade individuals from seeking essential medical care. In conjunction with public and private finance, charitable contributions and private donations exert a notable influence, particularly within the realm of voluntary healthcare. These contributions play a crucial role in providing essential support for certain medical programmes and research endeavours.
The government continues to prioritise capital investment, as seen by its inclusion of healthcare infrastructure development plans in the National Development Plan (Adshead et al., 2019). The investments encompass the establishment of novel healthcare facilities, improvements to pre-existing ones, and the procurement of cutting-edge medical technology with the aim of augmenting the calibre of healthcare services. In addition, it is worth noting that Ireland's healthcare initiatives might potentially secure financial support from the European Union, thereby emphasising the nation's dedication to enhancing its healthcare sector through international cooperation and financial resources.
The central focus of healthcare financing in Ireland is around the Sláintecare plan, a comprehensive initiative aimed at transitioning the country towards a universal healthcare system (Burke et al., 2021). This plan envisions a healthcare model wherein the funding for access to care is predominantly derived from general taxes. The primary objective is to guarantee the equal distribution of healthcare services, prioritising need over an individual's financial means. This objective aligns with the larger purpose of providing accessible healthcare to all members of society.
The cornerstone of healthcare procurement in Ireland is the Health Service Executive (HSE), which is in charge of the careful acquisition of supplies and services that support the provision of social and health care services (Sheerin, 2019). Privacyshield.gov, (2022) depicted that, since the HSE is the nation's largest buyer, with an annual procurement budget of almost €4 billion, procurement practices must be strict and heavily regulated within the parameters of intricate EU and national laws.
The HSE's procurement goals are centred on its steadfast dedication to ensuring the continuous provision of healthcare services (World Health Organization. Regional Office for Europe et al., 2019). This entails making certain that premium products and services are available exactly when and where they are required. In order to uphold the highest levels of ethics and openness, the HSE carefully complies with all legal requirements, legislative directives, circulars, and procurement directives. Compliance and governance are of utmost importance (Jeebhay et al., 2023).
A major component of the HSE's procurement strategy is value for money. Making every euro spent on healthcare procurement matter is the aim in order to reduce costs and reallocate funds to better patient care and services. Strategic and coordinated purchasing practises that increase compliance and efficiency are required under this approach. Notably, the HSE is aware of how procurement may advance social, economic, and environmental goals (Manutan, 2022). This involves encouraging social inclusion, supporting innovation, adhering to environmentally conscious practises, and encouraging small and medium-sized businesses (SMEs) to actively participate in the procurement process.
The HSE manages a suite of shared services capabilities that control the whole procurement lifecycle in order to expedite these crucial procurement endeavours. These functions—which range from sourcing and contracting to corporate procurement planning, logistics and inventory management, compliance enhancement, and business systems support—altogether guarantee that Ireland's healthcare procurement process is not only effective but also in line with the larger objectives of social cohesion, economic expansion, and environmental sustainability (Swords, 2021). In the end, this contributes to the ongoing improvement of healthcare services throughout the country. Planning for Corporate Procurement and Enhancing Compliance: In addition to managing procurement relationships,improving compliance, and building capabilities and capacities across a range of healthcare entities including Hospital Groups, Community Healthcare Organisations (CHOs), Section 38 and 39 Agencies, and
Corporate Services this unit also coordinates multi-annual procurement planning (Stepovic et al., 2020).
Decision-makers need to have access to economic evaluations of mental health therapies because they offer valuable information about how cost-effective different treatment options are. These assessments are especially important in Ireland because mental health issues have a substantial financial impact there, costing the country €11 billion a year. The loss of productivity in the labour market is mostly responsible for this economic burden, which highlights the significance of effective and efficient mental health therapies.
According to a noteworthy study conducted in this regard, there is a 0.77 chance that an early intervention will be cost-effective, meaning that it will probably have a favourable cost-benefit ratio. (Jeebhay et al., 2023). This indicates that a treatment programme is deemed cost-effective if its cost is less than €45,000 for each QALY achieved. Non-drug interventions fall under a separate cost-effectiveness threshold. Examples of non-drug interventions include different psychological therapies and other types of mental health support. The barrier in this instance usually lies between €20,000 and €45,000 per QALY. Cost-effective non-drug interventions are those that fall into this range (McGrath et al., 2022).
When it comes to choosing which healthcare interventions to implement, these thresholds are extremely important. They aid in determining the most effective way to distribute resources and assisting legislators and healthcare professionals in evaluating the financial sustainability of various mental health initiatives (Funk et al., 2008). Ireland can efficiently manage healthcare expenditures and promote the well-being of its residents while addressing the societal and economic problems caused by mental health difficulties by undertaking economic evaluations and taking these thresholds into account (Thomas and Chalkidou, 2016).
Over time, Ireland's Health Technology Assessment (HTA) framework-based economic evaluation rules for medical technology have expanded to include a wide range of health interventions. These recommendations offer a thorough and empirically supported method for evaluating the impact and cost-effectiveness of different healthcare technologies, ranging from prescription drugs to diagnostic equipment and public health initiatives. The Health Service Executive (HSE), on behalf of the publicly funded health and social care system, guarantees that assessments are in line with the Irish healthcare environment. Furthermore, including both the duration and quality of life, Quality-Adjusted Life Years (QALY) is the recommended outcome measure that reflects the overall impact of therapies. To overcome uncertainty in the evaluations, deterministic and probabilistic sensitivity analyses are carried out. Additionally, the dedication to fairness and equity in outcome metrics guarantees that healthcare interventions are beneficial to all populations. These recommendations represent Ireland's commitment to thorough and inclusive economic analyses, which will ultimately help the healthcare industry make well-informed decisions.
Public health and social justice intersect with healthcare equity and distribution. Fundamentally, the distribution of medical resources, services, and benefits among a population is the focus of healthcare distribution. This entails assessing the infrastructure such as clinics and hospitals that is available and making sure that medical professionals such as nurses and doctors are distributed appropriately. But distribution alone is insufficient; the distribution's quality is critical (Carroll et al., 2021). That's the point at which equity matters. Access to medical services should be determined by each patient's unique needs rather than by unrelated variables like gender, colour, income, or place of residence. This is known as equity in healthcare.
For instance, although there may be fewer healthcare facilities in rural areas, the needs of the people who live there are just as vital as those in urban ones. Similar institutional hurdles to healthcare may exist for historically marginalised populations; it is both morally and practically necessary to eliminate these barriers (Carroll et al., 2021). If these gaps are not addressed, the system runs the danger of exacerbating health disparities and resulting in worse health outcomes for the general public. Untreated illnesses or ailments can also raise long-term healthcare expenses and reduce productivity from an economic standpoint. Therefore, addressing healthcare fairness makes sense from an economic and policy standpoint in addition to being a matter of justice. Strategies including community engagement initiatives, universal health coverage, and ongoing data gathering to track inequities are crucial in achieving this goal (Biswas et al., 2022).They guarantee that everyone may get the treatment they require, irrespective of their circumstances or background, encouraging a more inclusive and healthy community.
Performance and health outcomes are crucial indicators of a healthcare system's efficacy. Health outcomes in Ireland are influenced by a multitude of factors, ranging from systemic investments to lifestyle choices.
Lifespan expectancy: Ireland has one of the highest rates of life expectancy in the EU. The life expectancy at birth was approximately 82 years as of the early 2020s, which is higher than the EU average (Ceeol, 2021). This is evidence of enhanced living standards, better healthcare, and lower mortality rates from serious illnesses.
Results of Disease:
Cardiovascular illnesses: Due to advancements in treatment and preventive measures, mortality rates from cardiovascular illnesses, such as ischemic heart disease, have declined over time, despite the fact that these conditions remain the primary cause of death (Jansen et al., 2022).
Cancer: Death rates from the disease have shown a variety of trends, with increasing survival rates for some varieties, such as breast cancer, attributable to improved detection and treatment. But in Ireland, cancer continues to be the primary cause of death (HMI, 2023).
Chronic lower respiratory disorders have been a source of concern, particularly for older people.
Healthy Practises:
Smoking: As a result of public health initiatives, laws, and raised awareness, the proportion of smokers in Ireland has declined over time. Smoking is still a serious threat to public health, though.
Drinking Alcohol: Ireland has one of the highest rates of alcohol use in the EU, which has consequences for problems with public health and chronic illnesses (HMI, 2023).
Obesity: As obesity rates rise, conditions like diabetes and heart disease may become more difficult to treat.
Access to Healthcare:
Although Ireland's healthcare system offers usually excellent care, there have been problems with access. There have been concerns raised about waiting times in the public healthcare system, particularly for specific treatments and surgeries (Connolly and Wren, 2019).
To address these issues, programmes such as Sláintecare have been introduced, emphasising prompt access to high-quality care based on need rather than financial means.
Mental Wellness:
With rising awareness and service funding, mental health has received more attention. There are still issues, though, particularly with relation to getting prompt care and assistance.
Health Care Outlays:
Ireland's health spending as a percentage of GDP has changed throughout time, but it is still less than the EU average. The focus has been on efficiency and effectiveness, with the goal of accomplishing more with the resources at hand.
Safety and Quality in Healthcare:
Ireland has worked hard in the past few years to raise the standard and security of medical treatment (Colombo and Tapay, 2021). This includes actions to lower the rate of hospital-acquired infections, boost patient satisfaction, and raise the standard of care in community and hospital settings .
Patient Contentment:
Surveys frequently reveal that although patients are generally happy with the quality of care, worries regarding wait times and accessibility continue (Collins and Homeniuk, 2021).
Recommendations
Coordinated Care:
Improving integrated care pathways between community, secondary, and primary healthcare services is the recommendation. This can guarantee more seamless patient transfers and lessen the burden on emergency hospital services (Irishlifehealth.ie, 2022). A well-organised care route guarantees prompt interventions, minimises duplication of services, and improves patient satisfaction.
Digital Conversion:
It is advised to give telemedicine and e-health solutions top priority. In Ireland's rural areas and in circumstances when in-person consultations present difficulties, these digital interventions may prove efficacious. There is a clear acceptability and preparedness for digital health solutions given their quick adoption during the COVID-19 epidemic (Connolly and Wren, 2019). This can lessen the strain on physical healthcare facilities and cut down on waiting times.
Health Promotion Initiatives:
It is advised to carry out and broaden programmes that oppose smoking and binge drinking while also encouraging a balanced diet and regular exercise (Privacyshield.gov, 2022). Tackle behavioural risk factors head-on to lower the burden of chronic diseases and reap major long-term health benefits.
Putting Money Into Mental Health:
It is advised that funding for mental health services be increased, with an emphasis on early intervention and community-based supports (McGrath et al., 2022). Mental health concerns are becoming more well known in Ireland. Better outcomes and lower long-term healthcare costs can result from early intervention.
Conclusion
Ireland's population is comparatively young, with more than 40% of people under 30. Although being young offers potential for a vibrant workforce, it also necessitates investments in areas such as employment possibilities, education, and family assistance. The difficulty facing the country is treating ailments like diabetes, heart disease, and obesity that are linked to a certain lifestyle. Many health services are provided by Ireland's healthcare system, such as acute care, primary care, continuing care, and community care. This all-inclusive strategy comprises both public and private healthcare practitioners and serves a range of health requirements, from family welfare to mental health.
In addition to providing specialised services and quicker access to healthcare for those who can afford it, the private healthcare industry supplements the public system. The cohabitation of the two systems benefits the economy by generating jobs and drawing medical tourists, as well as the general quality and accessibility of healthcare. Ireland's healthcare system is notable for its large capital expenditures and healthcare costs, both of which have increased significantly in recent years. The government's emphasis on building out the healthcare infrastructure is a reflection of its dedication to enhancing accessibility and quality of care.
References
Task 1: Report This report explores the vital role of lay magistrates within the English justice system, detailing their...View and Download
Chapter 1: Introduction Get free samples written by our top-notch subject experts by taking assignment help online from Rapid...View and Download
Introduction Get free samples written by our Top-Notch subject experts for taking online Assignment Help...View and Download
Introduction Get Free Online Assignment Samples from UK's Best Assignment Help Experts to boost your academic...View and Download
Introduction Get free samples written by our Top-Notch subject experts for taking online Assignment Help services. Service...View and Download
Introduction Get expert support with an assignment helper focusing on tourism, social bodies, and sensory engagement to enhance...View and Download
